19 Mar Plantar Fasciitis
The most common reason patients seek podiatric care is for heel pain. This condition can be caused by a variety of factors. Including, entrapped nerves, metabolic disorders, arthritis and infections. By far the most common cause, accounting for 95% of all cases, is abnormal, repetitive stresses placed on the anatomic structures of the foot and leg resulting in injury and inflammation. This condition is known as plantar fasciitis.
The plantar fascia has several functions. It helps keep the small muscles of the foot in a compact and efficient package beneath the foot when full weight is bore. More importantly, it helps maintain the bones of the foot in an “arch” orientation. As body weight is transmitted down through the leg and ankle, the foot tries to maintain a triangle shape. The base of the triangle is the plantar fascia. The fascia must resist the force of the heel and arch bones to flatten out. The extent to which the arch flattens is dependent on how much the plantar fascia can support. Thus, during the normal course of walking, our plantar fascia is subjected to tremendous, repetitive forces.
To understand what is causing heel pain, an examination of the anatomy is necessary. The plantar fascia is a dense thin layer of tissue just beneath the skin on the sole of the foot. It is shaped like a triangle (blue lines), with the apex oriented towards the back of the foot.

Anatomic Orientation of the Plantar Fascia
Since the plantar fascia is shaped like a triangle, a great deal of force is concentrated at the heel. When too much strain is placed on the fascia, the area of greatest strain becomes inflamed. This inflammatory process leads to pain and swelling. This is often termed plantar fasciitis or heel spur syndrome. Over time, this condition may produce bone projections off the heel known as spurs. Often times, patients will come to the podiatrist’s office with heel pain wishing their “spurs” be removed. They believe the heel pain is caused by these bony growths, when in fact, the true reason for the pain is from inflammation of their plantar fascia. The heel spur has developed in response to the chronic irritation of the plantar fascia on the calcaneus (heel bone).
Signs and Symptoms
Patients present to the podiatrist’s office with chronic pain to the bottom of the heel. Usually, this pain has been present for weeks to months and they have delayed seeking treatment hoping the symptoms would subside. Terms such as a stone bruise or deep ache are usually used to describe the discomfort. The onset is usually gradual, with no recollection of an injury or accident.
Classically, the pain is worse when arising from rest. For example, the first few steps taken after waking in the morning or after a prolonged period of sitting can generate the most pain. Once the foot warms up, the heel pain may lessen. Swelling or puffiness on the inside of the heel may also be noticed.
Treatment
“Treatment targets the plantar fascia, not the heel spur, since it is the true source of the pain.“
For the vast majority of patients (90%), conservative treatment can eliminate their pain. But this does not happen overnight. Rare, are the cases where one visit to the Podiatrist can completely alleviate their symptoms.
We tailor our treatment to the individual patient, taking into account health, lifestyle and their work environment. A cookie cutter approach will not be as effective, as there are many factors which must be considered. In general, the steps outlines below are utilized in different combinations and varying degrees of emphasis.
Anti-inflammatory Medication:
Also known as NSAID’s, this class of drugs helps to decrease the inflammatory process which maybe occurring around the damaged plantar fascia. These medications should only be used for very short periods of time and the risks vs. the benefits must be weighed with each individual patient. Serious complications can occur using this class of medicine.
Stretching:
By stretching, if by far the most important part in the resolution of this condition. Stretching instructions are to be performed on a daily basis. Skipping this step and relying on medications alone will not result in a long term resolution. Night splints are also an integral part in stretching the plantar fascia, Achilles tendon and calf muscle.
Injections:
Injection into the plantar fascia of a long acting steroid provides potent anti-inflammatory action. They are used for moderate to severe cases of plantar fasciitis. Plantar fasciitis which does not respond to other forms of treatment is also an indication for injection therapy. Although no stead fast rule exist as to the number of injections you can receive, be aware the multiple steroid injections into the same anatomical area can result in permanent tissue damage.
Arch Supports:
These devices help to support the arch and take pressure off the plantar fascia. They are placed in shoe gear and can help prevent recurrence of the condition. Both, podiatrists prescribed custom molded orthotics and over-the-counter devices can be effective.
Shoe gear:
Proper fitting and supporting shoe gear is critical is alleviating heel pain. Many times we place our patients in athletic shoes for prolonged periods. These styles allow more support to the arch and heel, creating a favorable environment for recovery. Do not use flats while trying to recover from plantar fasciitis.
Rest:
In severe cases of heel pain, we ask our patient to take time off work to rest their foot. This is especially true for people who spend a great deal of time on their feet. This may be combined with immobilization in a short leg cast.
Surgery:
Surgery maybe needed for those cases of plantar fasciitis which have failed all forms of conservative treatment. There are many different forms of surgery for plantar fasciitis, each of our podiatric physicians has his preferred method.
I prefer to perform the EPF (endoscopic plantar fasciectomy) procedure. This procedure has a good success rate which has been proven in the medical literature. It is, however, not without some risks. Calcaneal-cuboid joint syndrome is a possible complication with any surgery where the plantar fascia is transected. Although rare, it does occur.
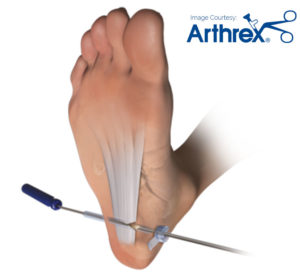



Intact Plantar Fascia

Transectioning of Plantar Fascia

Endoscopically Transectioned Plantar Fascia
Extracorporeal shock wave treatment (ESWT)
Dr. Strash was the first to offer this treatment in the San Antonio area. From the San Antonio Business Journal…
“Walter Strash has a solution for his patients suffering from heel spurs that is best described as shocking.
That’s because Strash is utilizing a state-of-the-art, non-invasive treatment for the heel condition that sends an electrical charge into the heel to remove the spur. The method has previously been used to treat kidney stones…Strash went to Atlanta to undergo training in the procedure, and in January 2001 began to offer it to his San Antonio patients.
“We’ve treated approximately 48 patients in the past seven months,” he says. “We have found one-third of the patients have 90 percent or greater rehabilitation between a three- to 12-week period.” Full story here.

This technology represents the latest innovation in the treatment of resistant plantar fasciitis. We have been utilizing this modality since January of 2000 with excellent results. It is performed in our podiatric office and does not require time off of work.

